Exams And Diagnostic Test For Renal Failure
 In the diagnosis of Renal failure, There are various sources tests as used That can be relevant to renal failure, includes:
In the diagnosis of Renal failure, There are various sources tests as used That can be relevant to renal failure, includes:1. Kidney function tests.
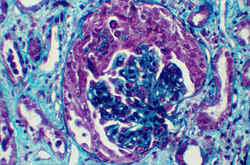
These are the diseases or medical conditions in which the medical test 'Kidney tests' may be involved: Diabetes, Hyperparathyroidis, Kidney stones, Renal osteodystrophy, Type 1 diabetes Wegener's granulomatosis.
2. Urine tests.
The urine may contain various substances for different types of disease. For example, sugar in urine may mean diabetes and blood in urine may mean various kidney conditions. Thus, a variety of diseases have urine tests.
There are several types of different urine tests;Fasting urine test, Random urine test, Mid-stream urine test, 24-hour urine test.
 3. Blood tests.
3. Blood tests.The blood laboratory tests used in the diagnosis of Renal failure, Such tests may include: BUN, Serum potasium, Creatinine clearance, Serum creatinine, Serum potassium, phosphorus, Urinalysis.
Blood tests may help reveal the underlying cause of kidney failure. Arterial blood gas and blood chemistries may show metabolic acidosis.
In a normal animal, the BUN is 25 or so. A good goal for BUN in renal failure is 60-80. Often at the time of diagnosis, BUN is well over 150, 200, or even 300.
A normal creatinine is less than 2.0. A good goal in renal failure is a creatinine of 4.5 or less. BUN and creatinine will be tracked (as will several other parameters) over time and in response to different treatments.
The calcium/phosphorus balance becomes deranged in renal failure due to hormone changes that ensue as well as the inability of the failing kidney to excrete phosphorus. If calcium and phosphorus levels become too high, the soft tissues of the animal's body will develop mineralized deposits which are inflammatory and uncomfortable. The bones will weaken as well.
If phosphorus can be maintained in the normal range (less than 7.5), a special medication called "calcitriol" can be used to help prevent or slow the progression of kidney failure. Medications and special diets can be used to help keep phosphorus levels down.
The failing kidney is unable to conserve potassium efficiently and supplementation may be needed. Signs of "hypokalemia" (the scientific name for low blood potassium) include weakness, especially drooping of the head and neck.
PACKED CELL VOLUME/HEMATOCRIT - This is a measure of red blood cell amount. More literally it represents the percentage of the blood made up by red blood cells. The hormone that stimulates the production of red blood cells is made by the kidney. The failing kidney does not make this hormone in normal amounts and anemia can result.
Anemia is often worsened by the extra fluid administrations needed to manage the kidney toxins. Sometimes a blood transfusion is needed or, more commonly, the owner of the pet must learn how to give hormone injections to boost the red blood cell count.
 Blood pressure is not something measured off a laboratory result sheet but it is important to monitor in kidney patients as there is a tendency for hypertension to develop in kidney failure. Special medications may be needed to manage this problem should it arise.
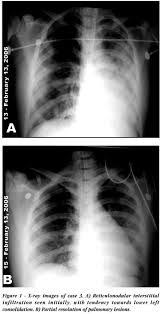
Blood pressure is not something measured off a laboratory result sheet but it is important to monitor in kidney patients as there is a tendency for hypertension to develop in kidney failure. Special medications may be needed to manage this problem should it arise.4. Radiology Tests.
A kidney or abdominal ultrasound is the preferred test for diagnosing kidney failure, but abdominal x-ray, abdominal CT scan, or abdominal MRI can tell if there is a blockage in the urinary tract.
5. Home Diagnostic Tests
Bladder & Urinary Health: Home Bladder Tests, Home Urinary Tract Infection (UTI) Test, Home Cystitis Tests, Home Kidney Tests, Home Urine Protein Tests (Kidney Function), Home Prostate Cancer Tests.
Renal Health: Home Microalbumin Tests (Kidney/renal), Home Urine Protein Tests (Kidney/renal), Home Urinary Tract Infection (UTI) Tests. Read more!















